Fatty liver disease, also known as hepatic steatosis, is a growing health concern in the United States, affecting millions of adults and even children. Characterized by excessive fat buildup in the liver, this condition can lead to serious complications if left untreated. This comprehensive guide explores the types, causes, symptoms, diagnosis, treatment, and prevention of fatty liver disease, incorporating recent data from U.S. government sources to provide a reliable and informative resource for American readers.
What is Fatty Liver Disease?
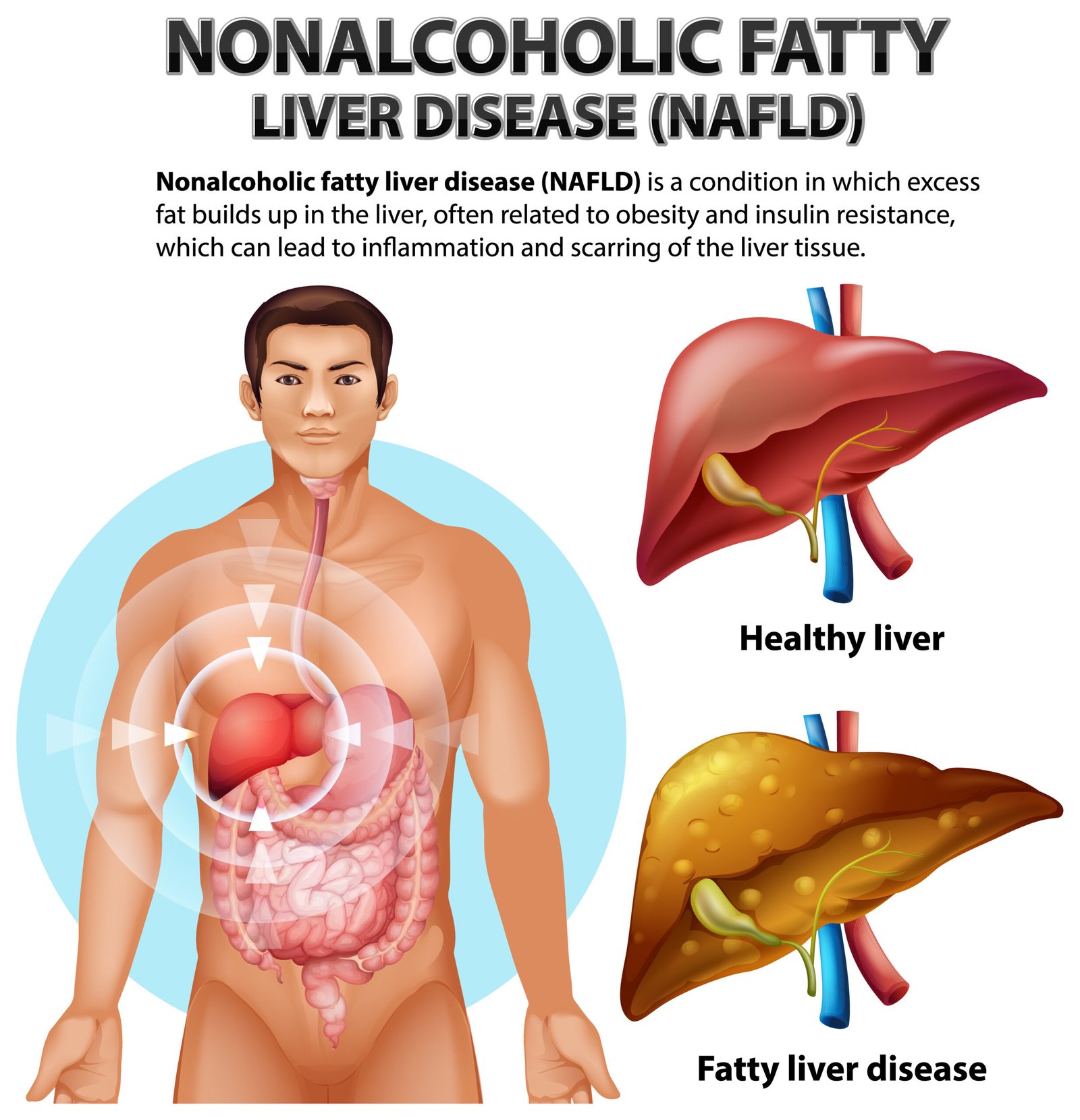
Fatty liver disease occurs when more than 5% of the liver’s weight is fat. It is broadly classified into two main types:
- Nonalcoholic Fatty Liver Disease (NAFLD): Now referred to as Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD), this type affects individuals who consume little to no alcohol. It ranges from simple fat accumulation (nonalcoholic fatty liver or NAFL) to a more severe form called Nonalcoholic Steatohepatitis (NASH) or Metabolic Dysfunction-Associated Steatohepatitis (MASH), which includes inflammation and liver damage.
- Alcoholic Fatty Liver Disease (AFLD): Caused by excessive alcohol consumption, this condition is an early stage of alcohol-associated liver disease (ALD). It is reversible with abstinence but can progress to alcoholic hepatitis or cirrhosis if drinking continues.
According to the National Health and Nutrition Examination Survey (NHANES) 2017–2018 data, approximately 42% of U.S. adults have some form of fatty liver disease, with MASLD being the most common, affecting about 42% of the population. Hispanic Americans face a higher prevalence at 47%, while Black Americans have the lowest rates.
Causes and Risk Factors:
Fatty liver disease is closely linked to lifestyle, genetic, and metabolic factors. Key causes and risk factors include:
Nonalcoholic Fatty Liver Disease (MASLD/NAFLD)
- Obesity: About 65% of overweight adults and 90% of those with severe obesity have MASLD. The obesity epidemic in the U.S., with 42% of adults classified as obese (CDC, 2017–2018), drives the rise in NAFLD.
- Type 2 Diabetes: Up to 70% of individuals with type 2 diabetes have MASLD, as insulin resistance promotes fat accumulation in the liver. The CDC reports that 13.0% of U.S. adults have diabetes, amplifying NAFLD risk.
- Metabolic Syndrome: Conditions like high blood pressure, high triglycerides, and low HDL cholesterol increase NAFLD risk. The NHANES 2013–2016 data estimates 31.9% of U.S. adults have NAFLD based on noninvasive markers.
- Genetics: Hispanic Americans have a higher genetic predisposition to NAFLD, partly due to variants like the PNPLA3 gene.
- Poor Diet: Diets high in ultra-processed foods, sugars, and saturated fats contribute to liver fat buildup. The USDA’s 2019 Economic Research Service notes that food insecurity, affecting 10.5% of U.S. households, correlates with poor diet quality and NAFLD risk.
Alcoholic Fatty Liver Disease (AFLD):
- Excessive Alcohol Consumption: Consuming more than 60 grams of alcohol daily (about 4–5 drinks) can lead to AFLD. The CDC’s 2021 Behavioral Risk Factor Surveillance System indicates that 5.4% of U.S. adults engage in heavy drinking, increasing AFLD risk.
- Chronic Alcohol Use: Prolonged drinking alters liver metabolism, favoring fat accumulation. Women are at higher risk of ALD-related mortality than men.

Emerging Risk Factors:
- Pediatric NAFLD: The Washington Post (2023) reports that pediatric fatty liver disease is as common as asthma in U.S. children, linked to maternal obesity, ultra-processed diets, and changes in infant formula.
- Environmental Factors: Exposure to certain chemicals may contribute to NAFLD, though more research is needed.
Symptoms and Diagnosis:
Fatty liver disease is often called a “silent” condition because it may present no symptoms, especially in early stages. When symptoms occur, they may include:
- Fatigue
- Discomfort or pain in the upper right abdomen
- Unexplained weight loss
Severe cases (NASH/MASH or advanced ALD) may cause jaundice, swelling, or confusion due to liver dysfunction.
Diagnosis Methods:
- Blood Tests: Elevated liver enzymes (ALT, AST) may indicate liver damage. The American Liver Foundation notes that routine screenings often miss NAFLD.
- Imaging: Ultrasound, CT, or MRI can detect liver fat. Transient Elastography (used in NHANES 2017–2020) measures liver fat (CAP > 300 dB/m) and stiffness (> 8 kPa), revealing 28.8% prevalence of fatty liver and 10.4% with fibrosis in the U.S.
- Liver Biopsy: Used for confirming NASH/MASH or staging fibrosis, though less common due to invasiveness.
- Noninvasive Scores: The U.S. Fatty Liver Index (US FLI) predicts NAFLD with an AUC of 0.80, showing a prevalence increase from 18% (1988–1991) to 31% (2011–2012).
Shockingly, only 7.2% of U.S. adults with fatty liver disease and 10.9% with fibrosis are aware of their condition, per NHANES data, highlighting the need for better screening.
Complications and Economic Burden:
Fatty liver disease can progress to serious conditions:
- Cirrhosis: Scarring of the liver, increasing the risk of liver failure.
- Hepatocellular Carcinoma (HCC): NAFLD is a growing cause of liver cancer, with a 3%–5% prevalence of NASH in the U.S. population.
- Cardiovascular Disease: NAFLD doubles the risk of heart disease, the leading cause of death in NAFLD patients.
- Liver Transplantation: NAFLD is now the second leading indication for liver transplants in the U.S., with 619 NASH-related transplants in 2014.
The economic burden is significant. A 2018 study estimated NAFLD costs the U.S. $32 billion annually, comparable to stroke ($34 billion). Long-term projections suggest $175 billion in NASH-related treatment costs over the next two decades.
Treatment and Management:
There is no FDA-approved medication for NAFLD/MASH, but lifestyle changes are effective. For AFLD, abstinence is critical.
Lifestyle Interventions
- Weight Loss: Losing 7%–10% of body weight can reduce liver fat and inflammation. The Mediterranean Diet, rich in fruits, vegetables, and healthy fats, is recommended.
- Exercise: 150 minutes of moderate aerobic activity weekly can improve liver health, even without weight loss. NHANES 2017–2020 found that individuals with fatty liver are less likely to meet physical activity guidelines.
- Diet Quality: Reducing sugar, refined grains, and seed oils while increasing omega-3 fatty acids (e.g., fish) helps. Posts on X highlight low-carb diets for NAFLD reversal.
- Alcohol Abstinence: For AFLD, stopping alcohol consumption reverses steatosis within 2–4 weeks.
Medical Management
- Managing Comorbidities: Controlling diabetes, cholesterol, and blood pressure reduces NAFLD progression.
- Emerging Therapies: GLP-1 agonists (e.g., Wegovy, Mounjaro) show promise for MASH by promoting weight loss and reducing liver scarring.
- Supplements: Some studies suggest vitamin E or pioglitazone for NASH, but results are inconsistent.
>>> Access USA Based Liver Support Supplement Here.
Screening and Early Detection
The American Liver Foundation’s Think Liver Think Life campaign aims to screen at-risk individuals in 50 states, targeting those with obesity, diabetes, or Hispanic/Asian descent. Early diagnosis is crucial to prevent progression.
Prevention Strategies:
Preventing fatty liver disease involves addressing its root causes:
- Maintain a Healthy Weight: Aim for a BMI of 18.5–24.9. The CDC’s Healthy Weight Program offers resources for sustainable weight management.
- Limit Alcohol: Follow CDC guidelines: ≤1 drink/day for women, ≤2 drinks/day for men.
- Healthy Eating: Prioritize whole foods and limit ultra-processed foods. The USDA’s MyPlate provides dietary guidance.
- Regular Screening: Adults with risk factors should request liver enzyme tests or imaging during annual checkups.
- Public Health Initiatives: Policies to reduce food insecurity and promote access to healthy foods can lower NAFLD rates.
USA Government Data Highlights:
- Prevalence: 42% of U.S. adults have fatty liver disease, with 47% of Hispanics affected (NHANES 2017–2018).
- Mortality: NAFLD-related mortality rose from 0.2 to 1.7 per 100,000 from 1999–2022, with a 10% annual increase (CDC WONDER).
- Economic Impact: NAFLD costs $32 billion annually, with hospitalizations increasing from 2007–2014 (HCUP-NIS).
- Pediatric Trends: NAFLD affects children as young as 2, mirroring adult obesity trends (CDC, 2021).
- Disparities: Women with ALD face higher mortality risk, and uninsured patients have worse outcomes (HCUP-NIS).
Conclusion:
Fatty liver disease is a silent epidemic affecting over 100 million Americans, driven by obesity, diabetes, and alcohol use. With 42% of U.S. adults impacted and many unaware, early screening and lifestyle changes are critical. Government data from NHANES, CDC, and HCUP underscore the urgency of addressing this public health crisis through targeted interventions, especially for high-risk groups like Hispanics and those with metabolic conditions. By adopting a healthy diet, exercising regularly, and limiting alcohol, individuals can prevent or reverse fatty liver disease, improving both liver and overall health.
For more information, visit the American Liver Foundation or CDC’s Liver Disease resources. If you’re at risk, consult a healthcare provider for screening and personalized advice.
Sources: National Health and Nutrition Examination Survey (NHANES), Centers for Disease Control and Prevention (CDC), Healthcare Cost and Utilization Project Nationwide Inpatient Sample (HCUP-NIS), American Liver Foundation, and peer-reviewed studies.

